Inflammatory bowel disorder in children
Written by the editorial staff writer at Hola. Medically Reviewed by Dr Nelson Lau, MBBS FRACGP, GP & Digital Health Specialist.

Contents

Summary: Inflammatory Bowel Disease (IBD), including Crohn’s and ulcerative colitis, causes persistent inflammation of the gastrointestinal tract. It leads to symptoms like stomach pain, frequent bowel movements, and impaired growth. Diagnosis involves tests and endoscopy, while treatment involves medications, nutritional management, and sometimes surgery. When children receive timely intervention and support, they can better manage their symptoms and maintain good health.
Inflammatory Bowel Disease (IBD) refers to a group of long-term digestive disorders marked by chronic inflammation in the gastrointestinal tract. The most prevalent forms are Crohn’s disease and ulcerative colitis, both of which can affect paediatric populations. IRecent studies indicate a rising incidence of paediatric IBD in Australia, particularly Crohn's disease, aligning with global trends. These disorders may cause severe symptoms and complications, potentially interfering with a child’s physical growth, development, and overall well-being. Understanding the causes, symptoms, and treatment approaches for IBD in children is crucial for effective care and better health outcomes.
What is Inflammatory bowel disease (IBD)
Inflammatory Bowel Disease is a chronic condition that causes swelling in the digestive tract. The primary types are Crohn’s disease, which can affect any part of the gut, and ulcerative colitis, which affects only the colon and rectum. IBD symptoms vary depending on the disease type and location but commonly is associated with symptoms such as abdominal pain, fatigue, weight loss, and diarrhoea. It is different from Irritable Bowel Syndrome (IBS), which does not involve inflammation or damage to the digestive system.What are the first signs of IBD in children?
Common early signs of IBD include:- Abdominal pain
- Diarrhoea
- Fatigue
- Loss of appetite
- Weight loss
- Poor growth
- Joint pain or swelling
- Fever
- Blood in stool
Also read: What are the symptoms of an IBS flare-up? A doctor’s guide
Experiencing these symptoms? Speak with a doctor within 15 minutes.
How is inflammatory bowel disease diagnosed in children?
Diagnosing Inflammatory Bowel Disease in children involves several steps because its symptoms often overlap with other health issues. Here’s how IBD is typically diagnosed in children:- Medical history and physical exam: The doctor begins by reviewing symptoms, family history, and physical signs of IBD.
- Blood tests: Blood tests assist in identifying signs of inflammation or anemia, which are often observed in IBD. These tests can also detect nutritional deficiencies, dehydration, and signs of infection.
- Stool tests: Stool tests are conducted to exclude infections or other gut conditions that could cause similar symptoms, like bacteria, viruses, or parasites.
- Endoscopy and colonoscopy: These are important diagnostic tools. A colonoscopy uses a flexible tube with a camera to inspect the large intestine and rectum. For Crohn’s disease, doctors may use an upper endoscopy or capsule endoscopy to view the small intestine. During these procedures, the doctor may obtain biopsies (tissue samples) to confirm the diagnosis.
- Imaging tests: Imaging techniques like X-rays, CT scans, or MRIs may be used to visualise the gastrointestinal tract, detect swelling, and check for complications like strictures (narrowing of the intestines) or abscess formation.
Types of IBD
Inflammatory Bowel Disease (IBD) in children primarily consists of two chronic illnesses: Crohn’s disease and ulcerative colitis. Both conditions lead to inflammation of the digestive system but target different areas and exhibit distinct characteristics.Crohn’s disease:
Crohn’s disease can impact any section of the gastrointestinal tract, from the mouth to the anus, but it predominantly affects the terminal part of the small intestine and the beginning of the large intestine. It is transmural, affecting all layers of the bowel wall and the inflammation may often penetrate deeply into the bowel wall. In children, Crohn’s disease can result in symptoms such as abdominal pain, diarrhoea, tiredness, weight loss, and delays in growth or puberty.Ulcerative colitis:
Ulcerative colitis only impacts the large intestine (colon) and rectum. In contrast to Crohn’s disease, the inflammation is continuous and confined to the inner lining of the colon. Children suffering from ulcerative colitis might have bloody stools, experience an urgent need to use the restroom, feel abdominal discomfort, and face growth delays.Indeterminate colitis:
At times, it can be challenging to differentiate between Crohn’s disease and ulcerative colitis in children. In these instances, the condition may be categorised as indeterminate colitis. This classification may evolve as additional symptoms arise, or further testing is conducted.Recognising the various forms of IBD in children—Crohn’s disease, ulcerative colitis, and indeterminate colitis is crucial for prompt diagnosis and effective treatment. Although managing these conditions can be demanding, with appropriate medical care and support, most children can control their symptoms and enjoy active, healthy lives.
Also read: Irritable Bowel Syndrome (IBS) symptoms: 12 foods to avoid
Causes
The precise cause of inflammatory bowel disease in children remains unclear, but it is thought to result from a blend of genetic, environmental, and immune system factors.
- Genetics: Children with a family history of IBD have a higher likelihood of developing the condition. Specific genes may render a child more prone to abnormal immune reactions in the gut.
- Immune system response: IBD may develop when the immune system incorrectly attacks healthy cells in the digestive tract, perceiving them as threats. This persistent immune response culminates in inflammation and damage over time.
- Environmental factors: Elements such as diet, gut microbiota, infections, and exposure to certain medications (like antibiotics during early childhood) may contribute to triggering IBD, particularly in genetically predisposed children. While these factors do not directly cause the illness, they may influence its initiation or exacerbations.
Although a singular cause for IBD in children is not identified, it is apparent that genetics, immune system dysfunction, and environmental elements all contribute. Comprehending these factors enables parents and healthcare professionals to collaboratively manage the condition early and effectively, providing children with the best prospects for a healthy, active life.
Diagnosis
Diagnosing IBD in children entails reviewing medical history, conducting physical examinations, performing laboratory tests, and utilising imaging studies. Since symptoms can overlap with other digestive disorders, a comprehensive assessment is vital.
- Medical history and physical exam: The doctor will start by inquiring about the child’s symptoms, growth trends, a family history of IBD, and any prior health concerns. A physical examination can help detect abdominal tenderness, growth delays, or weight loss.
- Blood and stool tests: Blood tests can indicate inflammation, anemia, or nutritional deficiencies. Stool samples are frequently analysed to exclude infections and assess for inflammation in the digestive tract.
- Endoscopy and colonoscopy: These techniques enable doctors to directly visualise the interior of the digestive tract using a thin, flexible tube fitted with a camera. They can also obtain small tissue samples (biopsies) to confirm inflammation and differentiate between Crohn’s disease and ulcerative colitis.
- Imaging tests: Additional imaging techniques, like MRI or ultrasound, may be utilised to investigate areas of the digestive system that are more difficult to access or to identify complications such as fistulas or abscesses, which occur more frequently in Crohn’s disease.
Diagnosing IBD in children necessitates a thorough approach that integrates medical history, physical examinations, laboratory tests, and specialised procedures like endoscopy. Timely and precise diagnosis is crucial for managing the condition and ensuring that children receive appropriate treatment for their specific type of IBD.
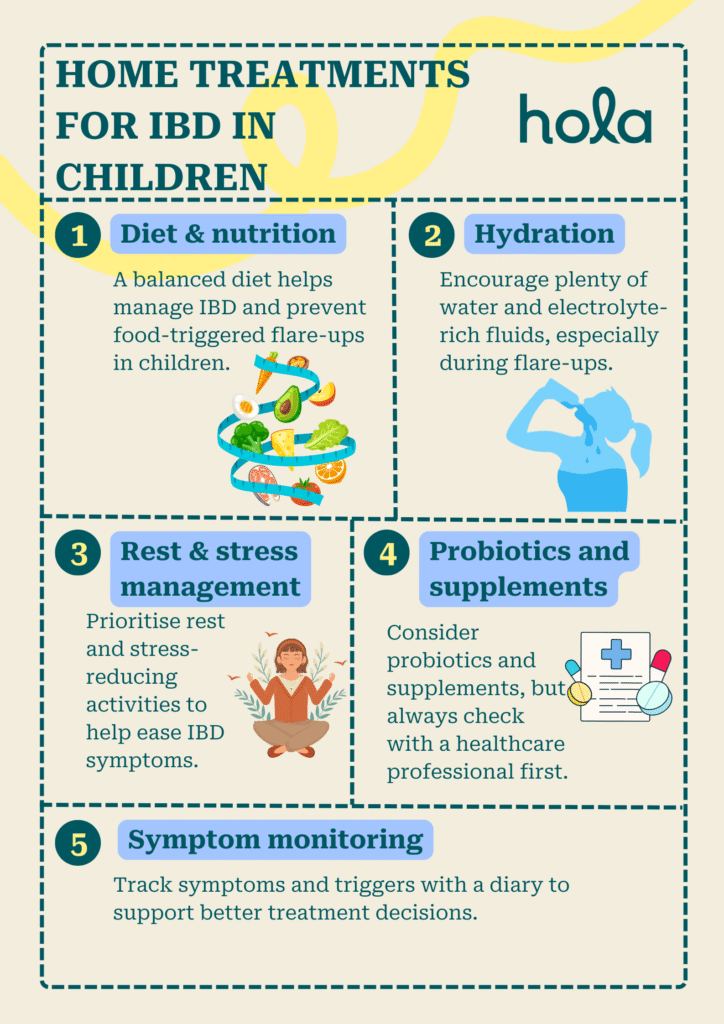
Home treatments
While medical intervention and professional support are vital in managing IBD, numerous home treatments and lifestyle modifications such as dietary medications under the guidance of a dietician can assist children with IBD in controlling their symptoms and enhancing their quality of life.
- Diet and nutrition: A properly balanced diet is vital for children with IBD. Certain foods might provoke flare-ups, so recognising and avoiding these triggers is essential. Collaborating with a dietitian can help develop a nutrition plan that guarantees sufficient calorie intake, especially if the child is facing weight loss or delays in growth. In some instances, specialised diets or nutritional supplements may be advised.
- Hydration: Maintaining hydration is vital, particularly during flare-ups when diarrhoea may lead to dehydration. Encourage the child to consume plenty of water and fluids rich in electrolytes to sustain adequate hydration levels.
- Rest and stress management: Ensuring enough rest and minimising stress can play a role in managing IBD symptoms. Stress is known to exacerbate flare-ups, so discovering ways to relax and de-stress, such as through hobbies, mindfulness practices, or gentle exercise, can be advantageous.
- Probiotics and supplements: Some parents may consider using probiotics and other supplements to promote gut health. Probiotics could help balance gut bacteria and alleviate symptoms in some children. However, it's important to consult a healthcare professional before introducing new supplements to confirm their safety and effectiveness.
- Monitoring symptoms: Keeping a symptom diary can aid parents in tracking flare-ups and identifying potential triggers. Observing changes in appetite, stool consistency, abdominal discomfort, or growth can assist healthcare providers in adjusting treatment plans as needed.
Home treatments for IBD in children, encompassing dietary modifications, hydration, stress management, and symptom monitoring, can significantly influence the management of the condition. While they should not replace professional medical care, these approaches can enhance daily comfort and well-being. It is essential to work closely with a healthcare provider to guarantee that home treatments support the prescribed medical plan.

Impact on growth and development
IBD in children can profoundly affect their growth and development, particularly in Crohn’s disease, where growth failure and delayed puberty are more prevalent compared to ulcerative colitis. Ongoing inflammation in the digestive tract can disrupt the body’s capacity to absorb nutrients, vital for a child's growth and overall advancement.
- Physical growth: Children with IBD, particularly those with Crohn’s disease, may undergo delays or slowed growth due to the malabsorption of crucial nutrients. This can lead to weight loss, hindered height growth, or postponed puberty. If not addressed, these growth delays may have lasting consequences on a child's physical development.
- Bone health: Prolonged inflammation from IBD, along with the use of medications such as steroids, can contribute to weaker bones or osteoporosis. Ensuring sufficient calcium and vitamin D intake, coupled with regular physical activity, can help safeguard bone health during treatment.
- Psychosocial impact: The emotional and psychological ramifications of IBD should not be overlooked. Children with chronic illnesses may face stress, anxiety, or depression associated with their symptoms or the lifestyle adjustments they need to make. The difficulties of managing a chronic condition can also influence social interactions and academic performance.
- Developmental milestones: Children with IBD may sometimes struggle to achieve specific developmental milestones, such as success in school or social integration, due to the physical and emotional hurdles they encounter. Early intervention with appropriate support systems can assist them in keeping pace with their peers.
IBD can influence a child's growth and development; however, with effective treatment and support, many children can manage the condition and continue to flourish. Timely intervention is essential to lessen these effects.
When to consult a GP
It is vital to consult a general practitioner if your child exhibits symptoms of IBD, including ongoing abdominal pain, diarrhoea, weight loss, or blood in the stool. Early consultation is important, particularly if symptoms are worsening or not improving with basic treatments. Furthermore, if your child experiences fatigue, stunted growth, or challenges in focusing, seeking medical advice is crucial. A GP can evaluate the symptoms, provide a referral to a specialist, and guide you through the subsequent steps for diagnosis and management.
How can telehealth with an online doctor help?
Telehealth with an online doctor offers several benefits for children with IBD and their families. It allows for convenient access to medical consultations without travel, making it particularly beneficial for those in remote locations or families with hectic schedules. Online consultations can assist with initial assessments, follow-up visits, and continuous management of treatment plans. During video calls, doctors can discuss symptoms, track progress, and modify the treatment plan as necessary. Telehealth also guarantees privacy and convenience, allowing families to consult healthcare providers from their own homes.
In addition, online doctors can give advice on symptom management, provide referrals to specialists, provide online scripts or valid medical certificates and help parents monitor their child’s health, especially when in-person visits are not immediately feasible.
In summary, IBD in children is a chronic condition that may influence a child’s health, growth, and day-to-day functioning. However, with early diagnosis, proper treatment, and consistent support from families and healthcare providers, most children can manage their symptoms and live active, healthy lives.
What we treat
- Cough
- Nausea & vomiting
- Fever
- Hayfever
- Fatigue
- Sore throat
- Acne
- Hair loss
- Gout
- Eczema
- Rosacea
- Sunburn
- UTI
- Erectile dysfunction
- Contraception
- Morning sickness
- Morning after pill
- Prostate health
- Anxiety
- Depression
- Stress
- Grief & loss
- Antidepressants
- Premature ejaculation
- Asthma
- Blood pressure
- Blood thinners
- Diabetes
- Cholesterol
- Migraines & headaches
- Allergies
- Body ache
- Heartburn & reflux
- Sleep disorder
- Pain relief
- Gastro
Related Articles
Disclaimer
This blog is for general informational purposes only and does not indicate that Hola Health provides all treatments or preventive measures mentioned. It is not intended to be a substitute for professional medical advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. For emergencies please immediately contact 000. Any medical topics discussed are intended to educate, not to imply availability through Hola Health.

Get affordable healthcare on your terms, with quick access to qualified, Australian-registered telehealth doctors & health practitioners, 24/7, 365 days a year. No more searching for ‘doctors near me‘ – Hola connects you instantly.
Address: 79 St Georges Terrace, Perth WA 6000


Hola Health App
Get affordable healthcare on your terms, with quick access to qualified, Australian-registered telehealth doctors & health practitioners, 24/7, 365 days a year. No more searching for ‘doctors near me‘ – Hola connects you instantly.
Call 000 for emergency or urgent medical help.
Address: 79 St Georges Terrace, Perth WA 6000
© Hola Health, a brand of Packapill Pvt Ltd

 Facebook
Facebook  X
X  Copy Link
Copy Link