8 Types of bipolar disorder: Understanding the differences
Written by the editorial staff writer at Hola. Medically Reviewed by Dr Nelson Lau, MBBS FRACGP, GP & Digital Health Specialist.

Contents

Summary: Bipolar disorder is a mental health condition characterised by intense shifts in mood. It exists in eight unique forms, each with distinct symptoms and patterns. These include Bipolar I, Bipolar II, Cyclothymic Disorder, along with variations involving rapid mood cycles, mixed episodes, or psychosis. Understanding these types is crucial for proper diagnosis and successful treatment. With appropriate care and support, individuals with bipolar disorder can manage their condition and live well.
Bipolar disorder is more than just occasional mood swings, it is a serious mental health condition marked by intense emotional highs and lows in mood, energy, and activity levels. What makes it even more interesting is that bipolar disorder isn’t just one simple mood swing; it has eight different types, each with its patterns and challenges. Recognising these variations is essential for proper diagnosis and treatment. In Australia, approximately 2.2% of the population (of Australians aged 16-85) is affected by some form of bipolar disorder, highlighting the need for greater understanding and support. Let’s explore the different types and what differentiates them.
What is bipolar disorder?
Bipolar disorder is a mental health condition marked by significant fluctuations in mood that encompass emotional peaks (mania or hypomania) and troughs (depression). During periods of mania, an individual may feel exceptionally energetic, self-assured, or irritable, and may partake in dangerous behaviours. In depressive phases, one might face feelings of sadness, reduced energy, and disinterest in everyday activities.
According to expert Aussie GP Dr Lau, mania lasts for at least 7 days (or less if hospitalisation is required), and hypomania lasts for at least 4 days. Psychotic symptoms, when present, occur during manic episodes or severe depression, not during hypomania.
These mood changes can affect sleep, energy levels, decision-making, behaviour, and clarity of thought. Managing bipolar disorder typically necessitates long-term treatment, incorporating medication and therapy, to help control symptoms and achieve stability.
Common symptoms: mania, hypomania, depression
The common symptoms of bipolar disorder differ based on whether an individual is experiencing mania, hypomania, or depression.- During manic episodes, signs include an excessively elevated or irritable mood, heightened energy, fast-paced speech, grandiose thoughts, a lesser need for sleep, impulsivity, or risky actions, and in some cases, hallucinations or delusions.
- Hypomania represents a less severe variant of mania. The indicators are comparable but less intense and usually do not cause significant disruptions in daily life. The individual may feel more productive, confident, and energetic while remaining grounded in reality. It is important to note that psychosis never accompanies hypomania.
- In the depressive state, symptoms encompass continual sadness, reduced energy, feelings of hopelessness, trouble focusing, alterations in appetite or sleep patterns, loss of enjoyment in activities, and occasionally thoughts of self-harm or suicidal ideation.
The main types of bipolar disorder
The primary categories of bipolar disorder consist of Bipolar I, Bipolar II, and Cyclothymic Disorder.- Bipolar I is defined by at least one manic episode, which can be severe and may necessitate hospitalisation. Depressive episodes often take place but are not essential for diagnosis.
- Bipolar II features episodes of hypomania, less severe than mania, along with significant depressive episodes. Individuals with Bipolar II generally face extended periods of depression.
- Cyclothymic Disorder is a milder, ongoing form involving episodes of hypomanic symptoms and mild depressive symptoms that persist for a minimum of two years but do not fulfil the complete criteria for manic or major depressive episodes.
- DSM-5 also describes bipolar-like conditions triggered by substances or medical illness, and ‘other specified/unspecified’ categories for presentations that don’t fit neatly into the main types.
Ready for positive change? Start your mental health care plan here.
Key differences between bipolar I and II
The primary distinction between bipolar I and bipolar II lies in the intensity of mood episodes. Bipolar I disorder entails at least one full manic episode, which is severe and can severely disrupt daily life or require hospitalisation. Depressive episodes may occur but are not necessary for diagnosis.
Conversely, bipolar II disorder includes hypomanic episodes that are less intense than full mania and usually do not lead to significant impairments. Nevertheless, bipolar II also involves one or more major depressive episodes that tend to last longer and may be more frequent than in bipolar I. Bipolar I is characterised by more extreme mood variations, while bipolar II has milder mania but often includes more severe depression. Hypomania also never leads to hospitalisation or psychosis, which is a defining feature.
Also read: Causes and effects of elderly social isolation
How bipolar disorder is diagnosed
Bipolar disorder is diagnosed through a thorough assessment by a mental health professional. This procedure typically consists of an in-depth review of symptoms, medical history, and any family history of mental health issues. The clinician will inquire about mood fluctuations, behavioural patterns, and how this impact daily living.
There is no blood test or brain scan that can confirm the diagnosis for bipolar disorder; hence, the diagnosis depends on clinical criteria specified in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). The clinician seeks evidence of manic, hypomanic, and depressive episodes persisting for specific durations.
At times, healthcare providers may eliminate other conditions that may produce similar symptoms, such as thyroid issues or substance abuse. A precise diagnosis is essential for developing an effective treatment plan, including medication and therapy to manage the disorder properly.
Managing bipolar disorder
Managing bipolar disorder involves a well-rounded strategy that merges medical care, therapy, and lifestyle modifications to stabilise mood and enhance overall well-being.- Medications: Mood stabilisers and antipsychotics play a crucial role in regulating mood fluctuations and diminishing episodes of mania or depression.
- Therapeutic support: Psychotherapy, especially cognitive-behavioural therapy (CBT), helps people understand their condition, recognise triggers, and develop effective coping strategies.
- Support network: Having a network of caring family members, friends, and mental health professionals offers emotional comfort and practical support during challenging periods.
- Lifestyle adjustments: Establishing consistent sleep routines, effectively managing stress, avoiding alcohol and drugs, and engaging in regular physical activity can all promote mood stability.
Also read: Alzheimer’s progression: The 7 key stages explained
Common treatments: medication, therapy, lifestyle
Typical approaches for managing bipolar disorder include medication, therapy, and lifestyle modifications. Medications typically involve mood stabilisers, antipsychotics, or antidepressants to regulate mood swings and avert episodes. Dr Nelson Lau, registered Doctor in Australia mentions that Antidepressants are generally second line and always combined with a mood stabiliser. Approaches such as cognitive-behavioural therapy (CBT) or psychoeducation help individuals comprehend the disorder and develop effective coping strategies. Lifestyle changes, including consistent sleep, stress management, depression treatment, abstaining from alcohol and drugs, and exercise, contribute to maintaining stability and enhancing overall health. The integration of these treatments provides the greatest likelihood of effectively managing symptoms.

When to consult a doctor
You should reach out to a healthcare provider if you experience ongoing mood swings that disrupt your daily activities, such as extreme highs or lows that persist for days or weeks. If you encounter symptoms such as heightened irritability, engaging in risky behaviours during manic episodes, or profound sadness and hopelessness during depressive phases, it’s crucial to seek medical attention. Sudden shifts in sleep, energy levels, or thought processes, along with any thoughts of self-harm or suicide, are urgent reasons to seek assistance. Seeking early help allows for accurate diagnosis and prompt treatment to manage symptoms effectively. Your GP can prepare a Mental Health Treatment Plan – either face-to-face or via telehealth under the Better Access scheme – before you are referred to a psychologist or psychiatrist. If you are in immediate danger, you can call Lifeline 13 11 14 or 000.
Conclusion:
Recognising the eight distinct forms of bipolar disorder helps ensure the right diagnosis and treatment. Each type has its challenges, but with increased awareness and support, people living with bipolar disorder can effectively manage their symptoms and enjoy meaningful, rewarding lives.
FAQs
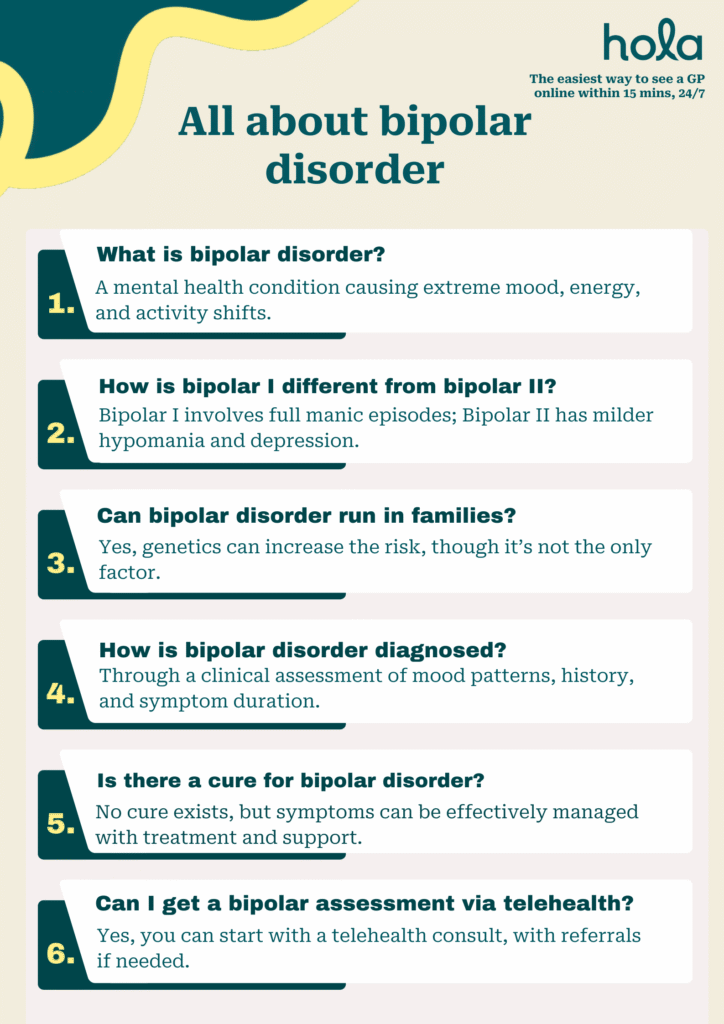
What is bipolar disorder?
Bipolar disorder is a mental health condition that leads to severe mood swings, ranging from emotional highs (mania or hypomania) and lows (depression). These shifts can influence a person’s energy levels, behaviour, thinking patterns, and ability to perform daily tasks. The mood changes may last for several days, weeks, or even longer, often interfering with personal relationships, work, and daily life. However, with the right treatment plan and support, people with bipolar disorder can manage symptoms and live a balanced, meaningful life.
What causes bipolar disorder?
Bipolar disorder results from a combination of various factors instead of just one specific cause. These factors include:
- Imbalances in brain chemicals or changes in brain structure
- Genetics
- Stressful life events, trauma, or abuse
- Irregular sleep patterns
- Drug or alcohol misuse
Is bipolar disorder genetic?
Yes, bipolar disorder can have a genetic component. It often runs in families, and having a close family member with the condition increases a person’s risk of developing it. However, genetics isn’t the only factor. Some people with a strong family history never experience the disorder, while others with no family history may still develop it.
How to diagnose bipolar disorder?
Bipolar disorder is diagnosed through a detailed assessment by a mental health specialist. This includes examining personal and family medical history, assessing mood patterns and behaviour, and sometimes using screening tools such as mood tracking diaries or questionnaires. Physical exams and laboratory tests may also be conducted to eliminate other possible causes. The diagnosis depends on the type, duration, and intensity of mood episodes, making it crucial to achieve an accurate diagnosis for effective treatment.
How to treat bipolar disorder?
Bipolar disorder is managed through mood-stabilising medications, therapy to address thinking patterns and emotional stress, healthy lifestyle habits, and support from loved ones or healthcare providers. Treatment is continuous and personalised, aiming to promote long-term stability and well-being.
What are the main types of bipolar disorder?
The main types of bipolar disorders and common specifiers that describe the course or features of bipolar disorder include:
- Bipolar l Disorder
- Bipolar ll Disorder
- Cyclothymic Disorder
- Bipolar Disorder with Mixed Features
- Bipolar Disorder with Rapid Cycling
- Bipolar Disorder with Psychotic Features
- Bipolar Disorder with Seasonal Pattern
Is there a cure for bipolar disorder?
No, there is currently no cure for bipolar disorder, but it can be effectively managed. With an effective mix of medications, counselling, healthy routines, and continued support, many individuals with bipolar disorder can lead stable, productive lives. Early diagnosis and regular treatment play a crucial role in easing symptoms, preventing relapses, and improving overall well-being. Stopping medication suddenly can significantly increase the risk of relapse.
What triggers bipolar episodes?
Bipolar episodes can be triggered by various factors, including:
- Stress
- Sleep disturbances
- Substance use
- Hormonal changes
- Medication changes
Triggers may vary from person to person, so recognising personal patterns can aid in managing the condition.
Can I get diagnosed with bipolar disorder through a telehealth consultation?
Yes, it is possible to start the diagnostic process for bipolar disorder through a telehealth consultation. A mental health professional can assess your symptoms, medical history, and emotional patterns remotely. However, for a complete diagnosis, they may suggest additional assessments, mood tracking, or referrals for in-person evaluation if necessary. Telehealth is a convenient and accessible starting point for getting support, Medical Certificates and treatment.
Take control of your mental health. Begin your care plan now.
What we treat
- Cough
- Nausea & vomiting
- Fever
- Hayfever
- Fatigue
- Sore throat
- Acne
- Hair loss
- Gout
- Eczema
- Rosacea
- Sunburn
- UTI
- Erectile dysfunction
- Contraception
- Morning sickness
- Morning after pill
- Prostate health
- Anxiety
- Depression
- Stress
- Grief & loss
- Antidepressants
- Premature ejaculation
- Asthma
- Blood pressure
- Blood thinners
- Diabetes
- Cholesterol
- Migraines & headaches
- Allergies
- Body ache
- Heartburn & reflux
- Sleep disorder
- Pain relief
- Gastro
Related Articles
Disclaimer
This blog is for general informational purposes only and does not indicate that Hola Health provides all treatments or preventive measures mentioned. It is not intended to be a substitute for professional medical advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. For emergencies please immediately contact 000. Any medical topics discussed are intended to educate, not to imply availability through Hola Health.

Get affordable healthcare on your terms, with quick access to qualified, Australian-registered telehealth doctors & health practitioners, 24/7, 365 days a year. No more searching for ‘doctors near me‘ – Hola connects you instantly.
Address: 79 St Georges Terrace, Perth WA 6000


Hola Health App
Get affordable healthcare on your terms, with quick access to qualified, Australian-registered telehealth doctors & health practitioners, 24/7, 365 days a year. No more searching for ‘doctors near me‘ – Hola connects you instantly.
Call 000 for emergency or urgent medical help.
Address: 79 St Georges Terrace, Perth WA 6000
© Hola Health, a brand of Packapill Pvt Ltd

 Facebook
Facebook  X
X  Copy Link
Copy Link