How to breathe easier with COPD: Effective strategies
Written by the editorial staff writer at Hola. Medically Reviewed by Dr Nelson Lau, MBBS FRACGP, GP & Digital Health Specialist.

Contents

Summary: Chronic Obstructive Pulmonary Disease (COPD) is a long-term lung condition that makes breathing difficult, but various effective strategies can help manage symptoms. Key strategies include quitting smoking, avoiding airborne irritants, and correctly following prescribed treatment plans. Breathing exercises such as pursed-lip and diaphragmatic breathing can improve airflow. Regular exercise, a balanced diet, and maintaining a healthy body weight also support better lung function. Preventing infections through vaccinations and hygiene, along with addressing stress and emotional well-being, further assists in easing respiratory difficulties. According to Dr Lau, registered GP in Australia, with appropriate medical care and lifestyle changes, people with COPD can often experience improved symptom control and enhanced daily functioning.
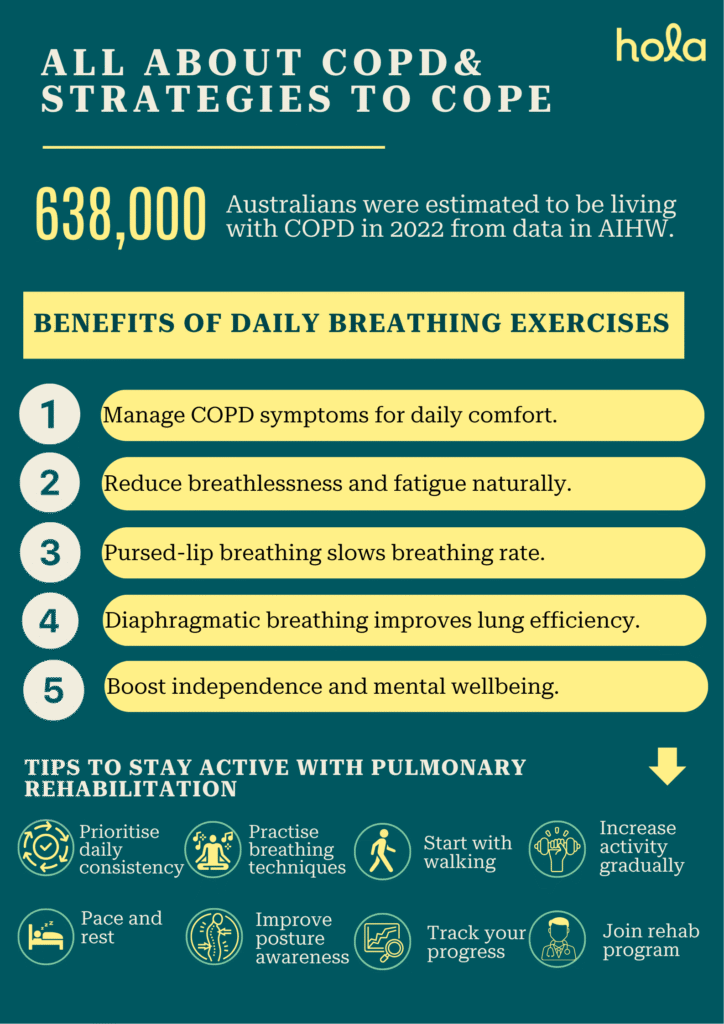
Chronic Obstructive Pulmonary Disease (COPD) is a chronic respiratory disorder that makes breathing difficult due to restricted airflow and lung tissue damage. In Australia, around 638,000 people, about 2.5% of the population, were estimated to be living with COPD in 2022. Although it can significantly affect everyday life, there are many effective strategies to manage symptoms and improve breathing, allowing those impacted to lead more active and comfortable lives.
Why does breathing become difficult with COPD?
Breathing becomes difficult with COPD because the bronchial tubes and alveoli in the lungs are damaged and constricted. This causes airflow obstruction, making it difficult to completely exhale air, leading to trapped air, inefficient gas exchange, and the sensation of breathlessness. Inflammation and excess mucus also worsen breathing difficulties by clogging the airways.Importance of symptom management for quality of life
Effectively managing symptoms in COPD is essential for enhancing quality of life, as it helps alleviate breathlessness, fatigue, and the frequency of exacerbations. Managing symptoms effectively helps individuals remain more active, achieve better rest, and maintain their independence, ultimately enhancing their overall well-being and mental health.Also read: Cough: COVID-19, flu, cold, RSV, or allergies – how to tell?
Experiencing these symptoms? Speak with a doctor within 15 minutes.
Benefits of daily breathing exercises
Breathing techniques can help individuals with COPD or other respiratory issues breathe more comfortably. Two effective methods are pursed-lip breathing and diaphragmatic breathing:- Pursed-lip breathing consists of inhaling slowly through your nose and gently exhaling through pursed lips (similar to blowing out a candle). This method helps slow down your breathing, keeps the airways open for a longer duration, and aids in releasing trapped air from the lungs.
- Diaphragmatic breathing (also known as belly breathing) emphasises using your diaphragm instead of your chest to take deeper breaths. You should place one hand on your chest and the other on your abdomen, and inhale so that your belly rises more than your chest.
Also read: Chronic cough: GP-approved management tips
How to stay active with pulmonary rehabilitation
Maintaining an active lifestyle is crucial for managing chronic lung conditions, and pulmonary rehabilitation provides a safe and structured way to achieve this. Here are key tips to help you stay active throughout the program:
- Begin with gentle, guided exercises such as walking, cycling, or stretching.
- Incorporate breathing techniques (such as pursed-lip or diaphragmatic breathing) during physical activity.
- Adhere to a structured pulmonary rehabilitation program supervised by healthcare professionals.
- Gradually increase your level of activity based on comfort and medical recommendations.
- Learn to pace yourself and take breaks to prevent overexertion.
- Emphasise consistency over intensity.
- Maintain proper posture to facilitate better breathing.
- Include basic strength training exercises to enhance endurance.
- Monitor your progress to stay encouraged.
Importance of light exercise in improving lung function
According to our medical expert- Dr Lau, while exercise does not reverse lung damage in COPD, it strengthens respiratory muscles and improves cardiovascular fitness, helping to reduce the sensation of breathlessness.
Gentle exercise is vital for enhancing lung health, particularly for individuals with chronic respiratory conditions like asthma or COPD. Activities like walking, gentle cycling, and stretching help to strengthen the muscles involved in respiration. When these muscles are stronger, your lungs work less hard, which alleviates feelings of breathlessness and fatigue. Moreover, regular physical activity improves circulation, increases oxygen distribution throughout the body, and enhances energy levels. It also promotes better breath control and boosts overall stamina, making routine tasks, such as climbing stairs or running errands, much less exhausting and easier to perform. Starting with light, regular exercise is generally more effective and sustainable than engaging in intense workouts for those managing lung issues.
What is pulmonary rehab, and how does it work
Pulmonary rehabilitation is a medically guided program designed to help individuals with chronic lung diseases improve their breathing and engage in more active lifestyles. It generally involves a team of healthcare specialists, including doctors, respiratory therapists, and physiotherapists, who develop a personalised treatment plan.
The program includes supervised exercise sessions to enhance physical fitness, breathing techniques like diaphragmatic or pursed-lip breathing to alleviate breathlessness, and education on lung health, nutrition, and symptom management. Emotional support and counselling are also provided to help reduce anxiety or depression that often accompany chronic illnesses.
Pulmonary rehabilitation is structured to gradually increase your strength and endurance in a safe, monitored environment. Over time, it can help decrease hospital admissions, enhance quality of life, and restore confidence in managing everyday activities.
Create a COPD-friendly home environment
Managing COPD involves establishing a home environment that facilitates easier breathing and minimises contact with irritants. Here are some methods to make your living space more suitable for those with COPD:- Minimise triggers: Ensure your home is free from typical irritants such as dust, smoke, and strong odours. Avoid using scented candles, air fresheners, or harsh cleaning substances. Make sure to ventilate the area properly when preparing food.
- Utilise air purifiers or humidifiers: An air purifier equipped with a HEPA filter can eliminate allergens and pollutants from the air. A humidifier helps maintain moisture in the air, particularly during dry periods, making breathing easier, however, humidifiers should also be used with caution, ensuring it’s regularly cleaned, and humidity levels are maintained between 30-50% to prevent mould growth, which itself can be a respiratory irritant.
- Keep medications and emergency plans accessible: Store inhalers and medications in convenient locations. Place a written emergency plan in a prominent spot, like the refrigerator or a bulletin board, so that everyone in the house knows the procedure during a flare-up.
Warning signs that symptoms are getting worse
For individuals with COPD, identifying early warning signs of deteriorating symptoms is essential to prevent serious complications. Look out for these changes:- Heightened shortness of breath, even at rest or with minimal activity
- Increased coughing or alterations in cough sound
- Wheezing or chest tightness that is new or worsening
- Alterations in mucus, such as increased production, a thicker consistency, or a change in colour (yellow, green, or bloody)
- Experiencing difficulty breathing while sleeping
- Lower energy levels or unusual fatigue
- Swelling in the ankles, feet, or legs, which may indicate fluid retention
- Fever or chills, which could signal an infection
When to consult a GP
You should reach out to a GP if you observe any changes in your COPD symptoms, such as worsening breathlessness, intensified coughing, changes in mucus, or chest tightness. It’s also crucial to seek medical guidance if your inhalers are not functioning as effectively as they usually do or if you find daily activities more challenging than before.
Other indicators that necessitate a GP visit include frequent flare-ups, fatigue that remains despite rest, or any symptoms of infection, such as fever or chills. Swelling in the legs or experiencing sleep disturbances due to breathing issues are additional reasons to seek medical attention. It’s advisable to have a COPD action plan prepared with your GP to guide you in responding to symptom changes.
If you are uncertain about the severity of your symptoms, it’s wise to be cautious; seeking early medical guidance can prevent complications. Book a telehealth appointment for asthma and breathing issues offer a quick and convenient way of obtaining support without leaving your home.
The benefit of regular check-ups and telehealth reviews
Regular check-ups and instant consultation with a doctor are vital for managing chronic illnesses like COPD. Regular check-ups often include spirometry to monitor disease progression and adjust your treatment plan accordingly, identifying issues early before they escalate. These appointments enable your doctor to assess lung function, review medications, and confirm that you are adhering to a care plan that is effective for you.
Through telehealth, you can book a telehealth appointment to obtain medical support from the comfort of your home, which saves time and minimises the risk of exposure to potential triggers such as pollution or infections. This method also simplifies maintaining consistency with follow-ups, asking questions, and receiving prompt assistance during flare-ups, including instant consultation with a doctor when needed. You can also request a medical certificate for COPD-related sick days if required. Together, both in-person and online appointments contribute to improved long-term health and help you manage your condition effectively.
Conclusion:
With the right treatments and healthy lifestyle adjustments, individuals with COPD can breathe easier and improve their quality of life. Small steps and strong support can have a meaningful impact.FAQs
What is the COPD medical abbreviation?
The medical abbreviation COPD stands for Chronic Obstructive Pulmonary Disease.What is COPD?
COPD, or Chronic Obstructive Pulmonary Disease, is a lung disease that causes airflow blockage and breathing difficulties. It includes illnesses such as chronic bronchitis and emphysema, leading to symptoms such as shortness of breath, coughing, and wheezing. COPD is usually triggered by prolonged exposure to harmful airborne irritants, especially smoking.How is COPD diagnosed?
COPD is diagnosed through a combination of medical history, clinical examination, and lung function tests. The key test is spirometry, which evaluates the amount and speed of air you can exhale. Healthcare professionals assess symptoms such as persistent cough and breathing difficulties, ask about smoking history or exposure to lung irritants, and may use chest X-rays or CT scans to eliminate other possible conditions. Early diagnosis can help manage COPD more effectively.What are the causes of COPD?
The main causes of COPD include:- Long-term exposure to irritants like air pollution, dust, or chemical fumes.
- Smoking
- Genetics
- Frequent respiratory infections
Can breathing exercises help with COPD?
Yes, breathing exercises can help people with COPD. Techniques such as pursed-lip breathing improve airflow and, ease breathlessness. These exercises improve your breathing efficiency, alleviate anxiety when experiencing breathlessness, and strengthen your respiratory muscles. While not a cure, regular practice of these exercises can make breathing easier and improve overall well-being.Is it safe to travel if I have COPD?
Yes, it is usually safe to travel with COPD, but it requires careful planning. It’s important to consult your healthcare provider before travelling to ensure your condition is stable and to receive personalised recommendations. Be sure to pack all the necessary medications, including inhalers or supplemental oxygen if prescribed and schedule time for rest during your trip. Avoid exposure to extreme weather, pollution, or infections, and know how to access medical care at your destination. With proper preparation, you can enjoy safe and comfortable travel.How often should I use my inhaler?
The frequency with which you should use your inhaler depends on its type and your doctor’s advice. Reliever inhalers are used only when needed for quick symptom relief, whereas preventer or combination inhalers are used daily to help manage symptoms and reduce the risk of exacerbations.Can I manage COPD entirely at home?
While you can manage many aspects of COPD at home, like taking prescribed medications, practising breathing techniques, avoiding irritants, and maintaining a healthy lifestyle, regular medical support is still important. COPD is a chronic and progressive condition, and regular check-ups with your doctor are important to monitor lung function, adjust treatment plans, and reduce the risk of severe exacerbations. Although daily care happens at home, ongoing medical supervision is essential for successful long-term management.Are there online GPs who can help with COPD management?
Yes, there are many online general practitioners (GPs) and telehealth services in Australia that can help with COPD management. These providers can:- Monitor symptoms and flare-ups
- Adjust medications
- Provide action plans for exacerbations
- Offer lifestyle advice
- Provide medical certificate online for sick leaves
- Provide specialist referrals for further checks
What we treat
- Cough
- Nausea & vomiting
- Fever
- Hayfever
- Fatigue
- Sore throat
- Acne
- Hair loss
- Gout
- Eczema
- Rosacea
- Sunburn
- UTI
- Erectile dysfunction
- Contraception
- Morning sickness
- Morning after pill
- Prostate health
- Anxiety
- Depression
- Stress
- Grief & loss
- Antidepressants
- Premature ejaculation
- Asthma
- Blood pressure
- Blood thinners
- Diabetes
- Cholesterol
- Migraines & headaches
- Allergies
- Body ache
- Heartburn & reflux
- Sleep disorder
- Pain relief
- Gastro
Related Articles
Disclaimer
This blog is for general informational purposes only and does not indicate that Hola Health provides all treatments or preventive measures mentioned. It is not intended to be a substitute for professional medical advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. For emergencies please immediately contact 000. Any medical topics discussed are intended to educate, not to imply availability through Hola Health.

Get affordable healthcare on your terms, with quick access to qualified, Australian-registered telehealth doctors & health practitioners, 24/7, 365 days a year. No more searching for ‘doctors near me‘ – Hola connects you instantly.
Address: 79 St Georges Terrace, Perth WA 6000


Hola Health App
Get affordable healthcare on your terms, with quick access to qualified, Australian-registered telehealth doctors & health practitioners, 24/7, 365 days a year. No more searching for ‘doctors near me‘ – Hola connects you instantly.
Call 000 for emergency or urgent medical help.
Address: 79 St Georges Terrace, Perth WA 6000
© Hola Health, a brand of Packapill Pvt Ltd

 Facebook
Facebook  X
X  Copy Link
Copy Link